Never make changes to your health protocol without your physcian’s explicit consultation.
My Approach to IBD & IBS
Mechanisms and Processes
An examination of the similarities and differences
By Andrew Kornfeld, BA, BS
Why I’m Writing This Post
As many of you know, I’ve been working diligently on the next iteration of IBDCoach, a transformative company set to address a multitude of chronic health conditions. Our mission is to fundamentally change healthcare systems, and we are set to launch next year. While our flagship program will continue to focus on the Inflammatory Bowel Diseases (IBD – Crohn’s disease, ulcerative colitis, indeterminate colitis, and microscopic colitis), we plan to expand to other gut-related conditions such as Irritable Bowel Syndrome (IBS), Small Intestinal Bacterial Overgrowth (SIBO), and diverticulitis shortly thereafter.
In the interim, I’ve been extremely fortunate since opening my personal coaching practice to be working with incredible new individuals with both IBD and IBS and I wanted to write a post to help demystify some of the differences between the conditions and illuminate the similarities – especially in the mechanism of action. This post will provide you a unique insight and may help you see your condition differently regardless of your diagnosis: IBD, IBS, or another lifestyle based condition.
Let’s dive in 👇
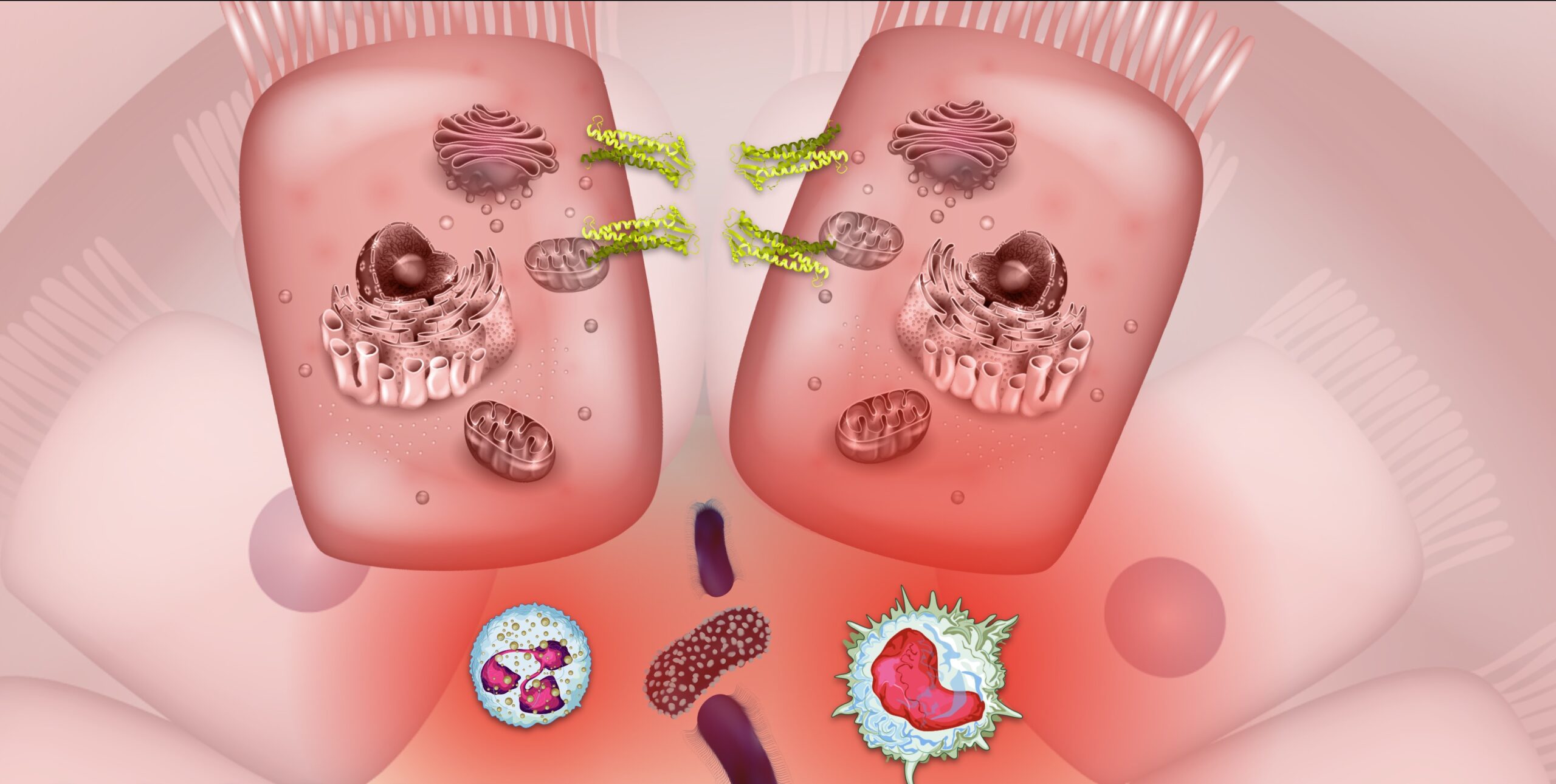
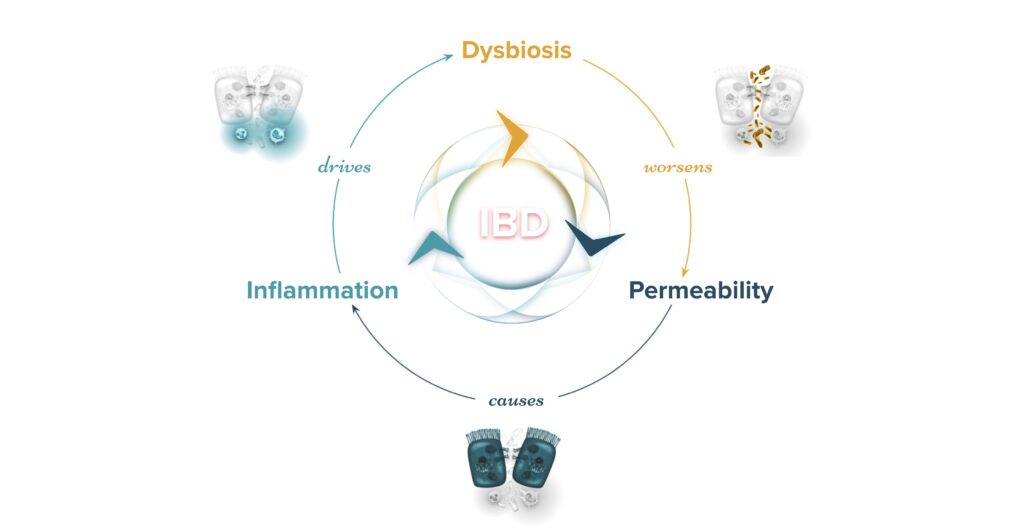
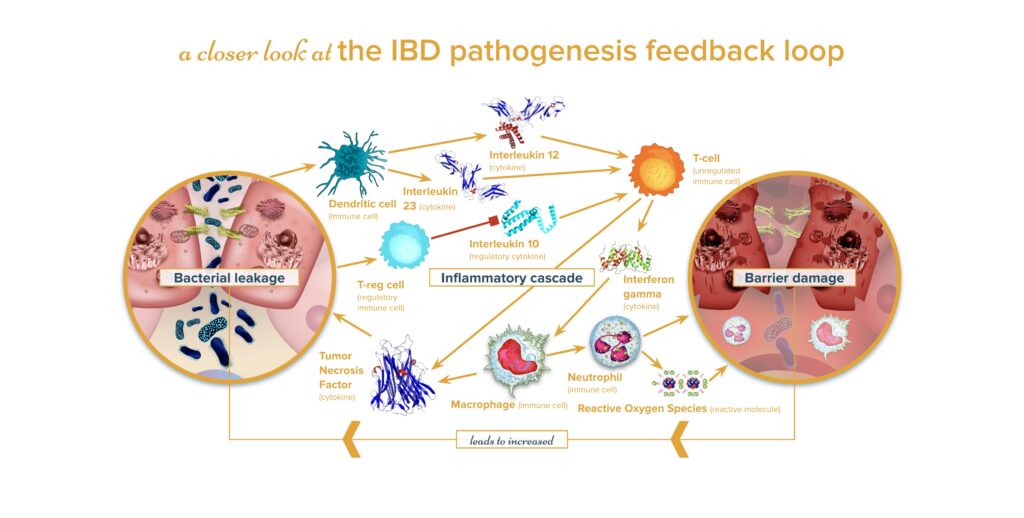
IBD Mechanism
In IBD, a combination of genetic, microbial (dysbiosis)[1–3], psychosocial, and other environmental factors contribute to the breakdown of the mucosal membrane. [4] This results in increased gut permeability [5,6] due to dysfunctional tight junction proteins, which are essential for holding the cells of the GI tract together. When microbes from the microbiota seep into the lamina propria (an area just beneath the first layer of cells), the body initiates an immune response (inflammation) [5] against these organisms. This isn’t an attack on the tissue itself; however, there’s collateral damage to the digestive tract in the process. In Crohn’s disease, this inflammation can manifest anywhere and is transmural, often appearing in the terminal ileum and colon. In contrast, ulcerative colitis affects only the most superficial layers, with inflammation exclusively located in the colon.


IBS Mechanism
Similar to IBD, factors such as genetics, microbes, psychosocial influences, and other environmental elements play a role in IBS. Additionally, there’s a believed increase in membrane permeability, possibly involving tight junction proteins, akin to IBD. There’s also an immune response, but the narrative shifts at this juncture. Instead of the immune activity leading to visible, physical lesions, this inflammation activates the Enteric Nervous System (ENS, which governs the gut). This, in turn, stimulates the Central Nervous System (CNS, comprising the brain and spinal cord), causing alterations in gut motility, changes in bowel movements, and visceral hypersensitivity (intense pain perception in the bowels). [7–9] These disturbances culminate in the signature symptoms of IBS: abdominal pain and variations in bowel movements. This can manifest as diarrhea (IBS-D), constipation (IBS-C), a combination of both (IBS-Mixed or IBS-M), or as undefined symptoms (IBS-U). [10]
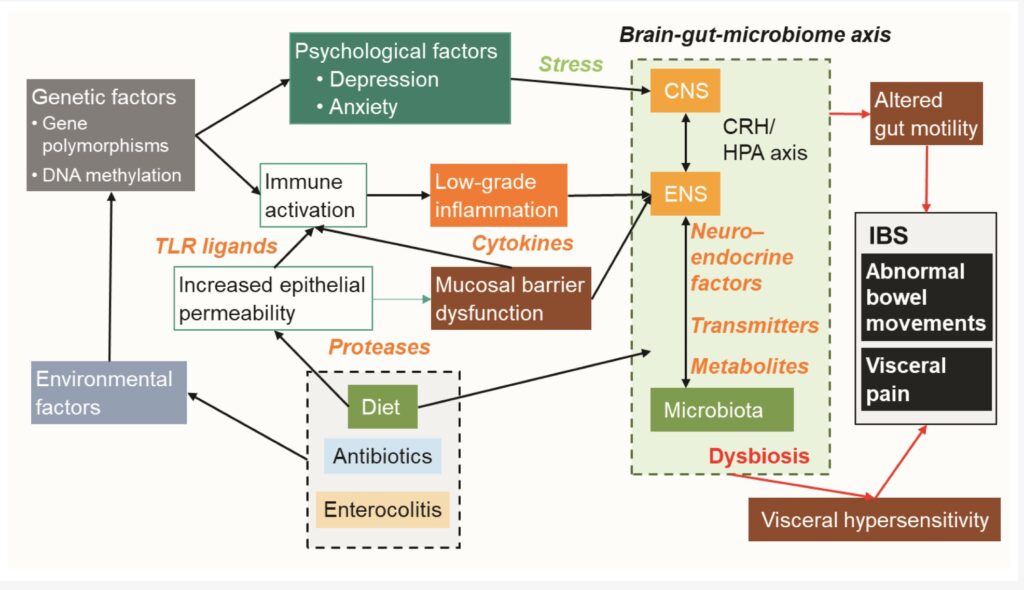
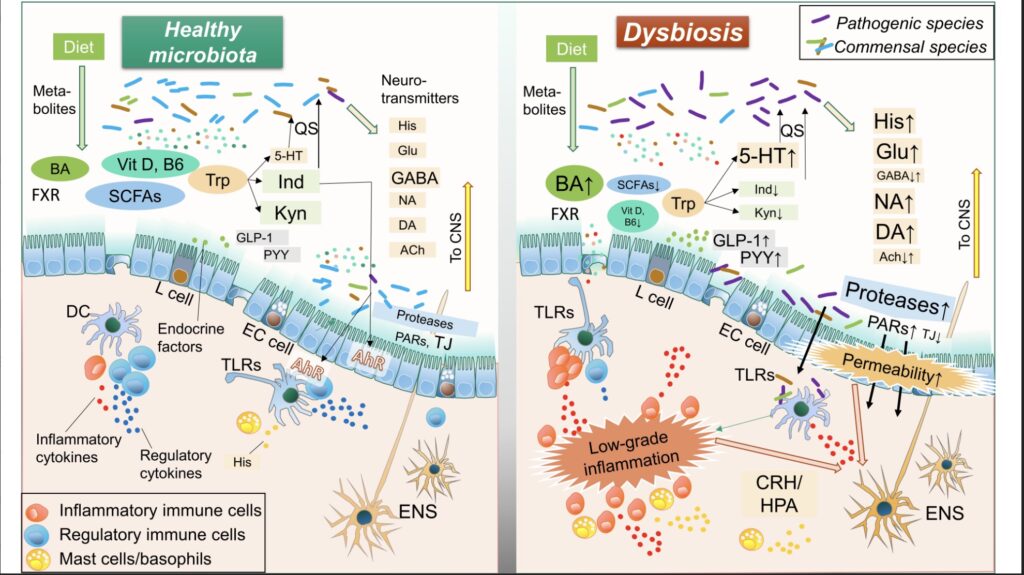
Figure Sources: Molecular Mechanisms of Microbiota-Mediated Pathology in Irritable Bowel Syndrome (open source article)
Approaching IBD and IBS
While both the ENS and CNS play significant roles in IBD, especially contributing to changes in bowel movements such as diarrhea, they play an even central role in IBS.
To simplify, I’ve delineated my processes for addressing IBD and IBS with this difference in mind:
3 Step Process to IBD
- Stop & Control Inflammation
- Modulate & Nourish the Microbiome
- Repair & Maintain the Barrier
(For a detailed approach, see our poster presented at the Crohn’s and Colitis Congress in 2022.)
4 Step Process to IBS
- Calm the Nervous System
- Modulate & Nourish the Microbiome
- Seal the Barrier
- Quell Inflammation
(I’ll soon release a microcourse on IBS that dives deeper into this, but for now, read more below.)
Inflammation
In IBD, it’s possible to halt inflammation using a multidimensional approach. In acute cases, corticosteroids often offer the quickest relief and can be the spark for lifestyle interventions (like diet, exercise, and mindfulness) to be a primary or secondary maintenance strategy. However, in the long run, in some cases other immunomodulatory, small-molecule medications and biologics can play an essential role. [11] It’s worth noting that I don’t see medications as “life-sentences,” but rather as strategic tools to control inflammation for specific periods. Countless foods and supplements, including vitamin D, [12] omega-3 fatty acids, [13] quercetin, [14] curcumin, [15] and other flavonoids and polyphenols found in tea, pomegranate juice, blueberries, [16,17] etc., can help modulate the immune system in IBD. It’s possible many of these agents can be beneficial in IBS (especially curcumin [18]), albeit in a more indirect manner and over extended durations, and additionally for prevention of flare ups. Modulating inflammation in IBS is an emerging concept and more research is needed in how to best address it. While there is less evidence in controlling inflammation directly in IBS with anti-inflammatory herbs and medicines, the role of inflammation is quite established and cannot be ignored. While the inflammation in IBD could be more related to the body’s over reactions to microbial translocations (leakage), the inflammation in IBS appears more strongly tied to the gut-brain axis and the enteric and central nervous systems.[19]
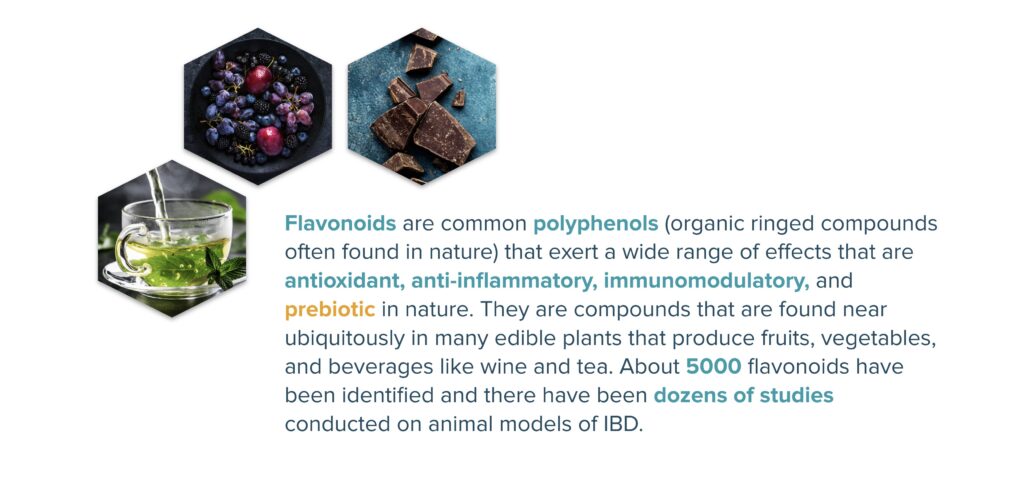
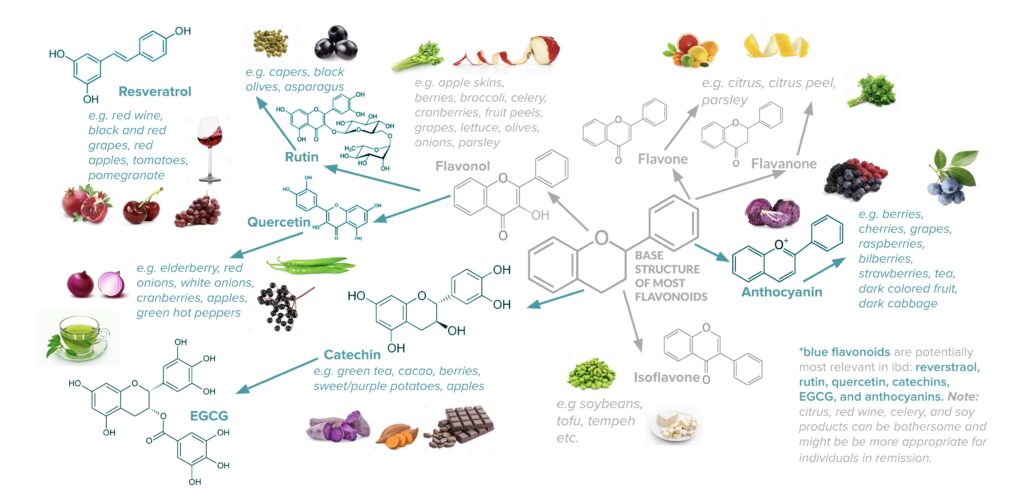
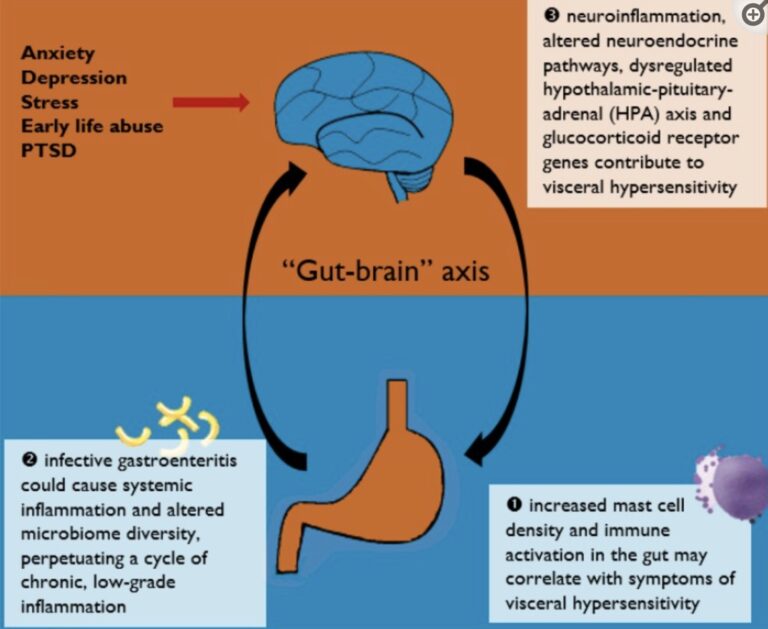
Figure Source: The Role of Inflammation in IBS (open source article)
The Microbiome and Dysbiosis
Distinct patterns of dysbiosis are evident in both IBS and IBD, with the latter displaying more pronounced deviations. [3] Fortifying the microbiome with prebiotics and probiotics is paramount for both conditions. [20–22] When opting for a microbiome supplement, especially a probiotic, it’s crucial to select one with proven efficacy for your specific condition and its subtypes. For instance, the dysbiosis patterns in IBS-D (diarrhea dominant) differ from IBS-C (constipation dominant), implying that the most beneficial probiotic may vary based on the subtype. Similarly, for IBD, the probiotic Visbiome (formerly VSL#3) offers no benefit for Crohn’s disease but proves effective for ulcerative colitis and proctitis for some individuals. [23] Personally, I prefer sourcing my probiotics from foods like kimchi, sauerkraut, yogurt (be it dairy or non-dairy), miso, and occasionally kombucha. It’s also vital to ensure adequate fiber and prebiotic intake from vegetables and fruits. Remember, these fibers undergo fermentation by intestinal bacteria, producing short-chain fatty acids (SCFAs) such as butyrate, which nourish colonocytes and assist in barrier repair. [24] Another point worth noting is that flavonoids and polyphenols, especially those found in dark berries, are among the few non-carbohydrate compounds that feed the microbiome. [17, 25] In IBD, dietary strategies like the specific carbohydrate diet (SCD), which reduces starchy complex carbohydrates, and in IBS, strategies that lower specific saccharides known as FODMAPs, may modulate the microbiome resulting in lower symptoms, inflammation, and visceral hypersensitivity. [26, 27] Based on my experience, these strict dietary interventions, akin to medications, aren’t permanent solutions. They’re more effective when used for specific periods before transitioning to long-term, sustainable strategies. In regards to microbiome testing one of my advisors, Dr. Lucy Mailing Ph.D. is currently one of the most pioneering and innovative voices in the microbiome and testing space. While most testing is generally more interesting than it is actionable, we have both found the Thorne microbiome test to be of potential benefit given that it provides the user with raw data down to the individual species of microbe in both IBD and IBS.
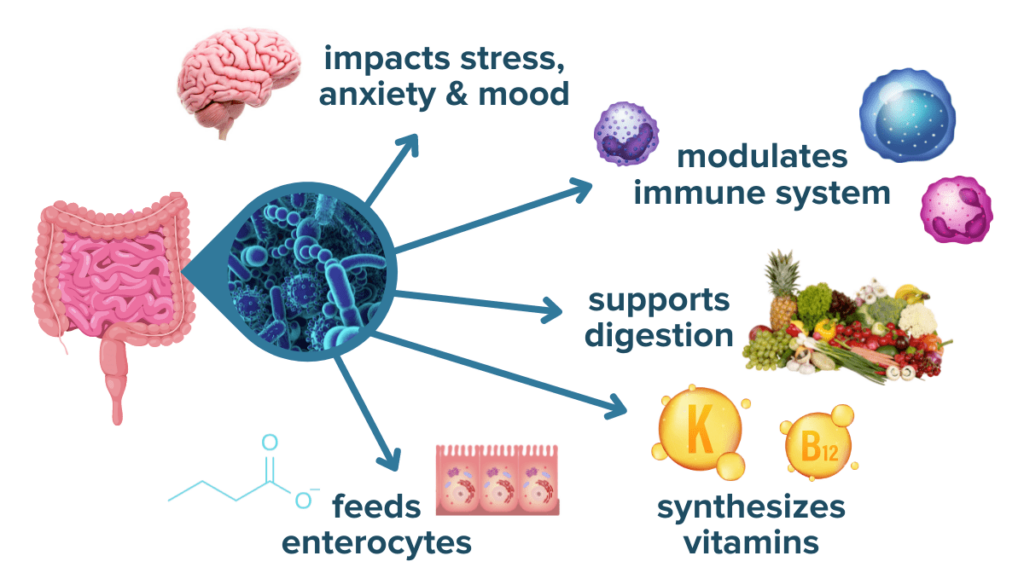
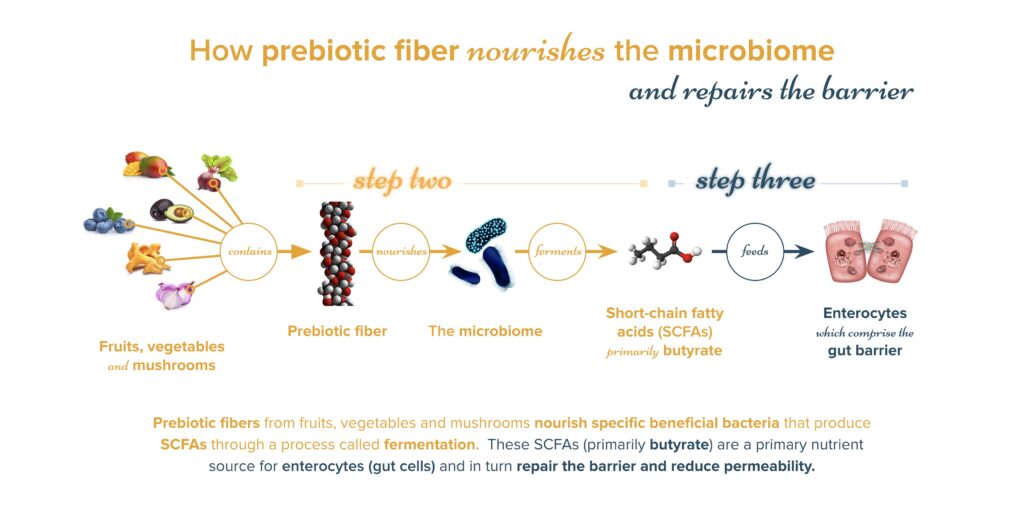
The Intestinal Barrier and Soothing the Gut
Both IBD and IBS show a leakage of bacterial and food particles, primarily due to dysfunctional tight junction proteins. While IBD showcases more damage to the intestinal lining, sealing this barrier and mending the lining remains essential. As mentioned, nourishing the microbiome, especially with gelatinous fermentable fibers (like blueberries, avocado, bananas) that lead to SCFA production, [24] is critical for sealing the barrier, considering their nutritional benefit to colonocytes. Supplements, including glutamine, [28] butyrate, [29] phosphatidylcholine, [30] Serum-derived bovine immunoglobulins (SBIs), [31] and herbs like marshmallow and slippery elm, [32–34] can be beneficial in both conditions, particularly in IBD. Lastly ginger and peppermint oil may show some gut soothing qualities in IBS. [35,36]

The Nervous Systems and Gut-Brain Axis
(also referred to as the Gut-Brain-Microbiome Axis)
My approach to IBD, grounded in systems thinking and neuroscience (particularly in activating neuroplasticity), places significant importance on the brain’s role. Activating plasticity allows individuals to reduce stress and stress hormones (like cortisol, which can disrupt the immune system) and, crucially, enables them to navigate the world, making lifestyle and food choices conducive to healing. In IBS, the CNS takes a more prominent role (as discussed earlier), making strategies like meditation, hypnotherapy, [37] and biofeedback [38] potentially scientifically valid for IBS treatment. The visceral pain and hypersensitivity in IBS stem directly from the interactions between the CNS and ENS. For meditation (in both IBD and IBS) the app Insight Timer (a non-profit company) is incredible, allowing for a lot of customization around silent practices or guided practices. I’ve also found the app Nerva which provides a hypnotherapy framework for IBS, to be useful; however I’m working on enhanced and more efficient protocols. Notably, vagal nerve stimulation shows promise in IBD treatment, interfacing directly with the gut-brain axis and thus may also play a role in IBS. [39,40]
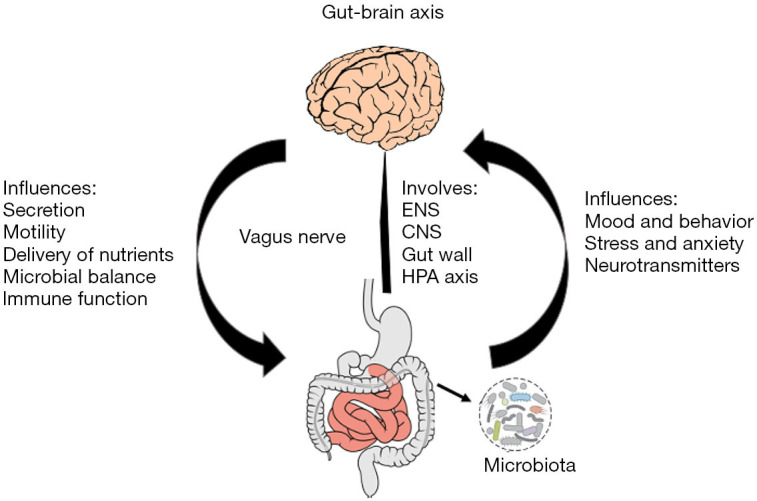
Figure Source: Uncovering the pathophysiology of irritable bowel syndrome by exploring the gut-brain axis: a narrative review (open source article)
Concluding Thoughts
You likely will not find a single silver bullet, but rather a multifaceted approach
This post is just scratching the surface of exploring the gut through understanding the similarities and differences between IBS and IBD. The fact remains that both conditions can be extremely debilitating. While IBD is objectively (in most cases) a more severe diagnosis, the diagnosis itself is more defined, while by contrast IBS is increasingly more broad and even more enigmatic. I’ve always believed what many gastroenterologists and researchers write in the literature: that IBD may encompass several dozen, even over a hundred subtypes. It’s likely IBS has even more.
I did not cover frontline medications for either condition in depth. However, there are several promising options for IBS-C, IBS-D and the IBDs. Most of these in IBS focus on addressing symptoms and some downstream functional problems while in IBD all medications work almost exclusively on inflammation. As you now know, the story is quite a bit more complex.
I’ve expanded my work to IBS and other chronic conditions (outside of just IBD) because IBS is more prevalent than IBD (about 10 times), there are significant overlap between the two conditions, and because by understanding both we can develop better overall theories of the gut, inflammation, microbiology, and the interaction with the nervous systems (primarily the CNS and ENS).
Regardless if you have IBD, IBS, or another gut-related or autoinflammatory/autoimmune condition, I’d love to work with you in applying my proven framework to your situation. Specific tools I utilize the like the Remission Master Plan (RMP) and the Adaptive Dietary Framework (ADF) are used nowhere else in the coaching industry or healthcare system. Working on a systems-based level addressing lifestyle, diet, supplements and herbs, medications, healthcare navigation, and mindset are vital to healing chronic health conditions of all types. Remember, it’s rarely one approach that will be your magic bullet. Rather, your key to success are multidimensional and coordinated interventions aimed at addressing you as a human being and building conducive environments.
When you’re in the depths of chronic illness, nothing matters but healing. Often an hour out of the day doesn’t go by without anxiety about your future. Learning to take control of these conditions is like learning a new language – this is the language of your body, of your health, and most importantly of your mind. Turning you into the human that perseveres is my number ONE job.
Let’s do it together. 🚀
Let's talk about your health
References
1. Glassner KL, Abraham BP, Quigley EMM. The microbiome and inflammatory bowel disease. J Allergy Clin Immunol. 2020;145(1):16-27. doi:10.1016/j.jaci.2019.11.003
2. Khan I, Ullah N, Zha L, et al. Alteration of Gut Microbiota in Inflammatory Bowel Disease (IBD): Cause or Consequence? IBD Treatment Targeting the Gut Microbiome. Pathog Basel Switz. 2019;8(3):E126. doi:10.3390/pathogens8030126
3. Sultan S, El-Mowafy M, Elgaml A, Ahmed TAE, Hassan H, Mottawea W. Metabolic Influences of Gut Microbiota Dysbiosis on Inflammatory Bowel Disease. Front Physiol. 2021;12:715506. doi:10.3389/fphys.2021.715506
4. Carreras-Torres R, Ibáñez-Sanz G, Obón-Santacana M, Duell EJ, Moreno V. Identifying environmental risk factors for inflammatory bowel diseases: a Mendelian randomization study. Sci Rep. 2020;10(1):19273. doi:10.1038/s41598-020-76361-2
5. Immunopathogenesis of inflammatory bowel disease and mechanisms of biological therapies. Accessed October 21, 2023. https://www.tandfonline.com/doi/epdf/10.1080/00365521.2018.1447597?needAccess=true
6. Michielan A, D’Incà R. Intestinal Permeability in Inflammatory Bowel Disease: Pathogenesis, Clinical Evaluation, and Therapy of Leaky Gut. Mediators Inflamm. 2015;2015:628157. doi:10.1155/2015/628157
7. Tang HY, Jiang AJ, Wang XY, et al. Uncovering the pathophysiology of irritable bowel syndrome by exploring the gut-brain axis: a narrative review. Ann Transl Med. 2021;9(14):1187. doi:10.21037/atm-21-2779
8. Mishima Y, Ishihara S. Molecular Mechanisms of Microbiota-Mediated Pathology in Irritable Bowel Syndrome. Int J Mol Sci. 2020;21(22):8664. doi:10.3390/ijms21228664
9. Shrestha B, Patel D, Shah H, et al. The Role of Gut-Microbiota in the Pathophysiology and Therapy of Irritable Bowel Syndrome: A Systematic Review. Cureus. 2022;14(8):e28064. doi:10.7759/cureus.28064
10. Rome IV Diagnostic Criteria for Irritable Bowel Syndrome (IBS). MDCalc. Accessed October 21, 2023. https://www.mdcalc.com/calc/4007/rome-iv-diagnostic-criteria-irritable-bowel-syndrome-ibs
11. Puckett S. Treatments for Inflammatory Bowel Disease | IBDCoach. Published January 15, 2022. Accessed October 22, 2023. https://ibd.coach/ibd-treatments/
12. Fletcher J, Cooper SC, Ghosh S, Hewison M. The Role of Vitamin D in Inflammatory Bowel Disease: Mechanism to Management. Nutrients. 2019;11(5):1019. doi:10.3390/nu11051019
13. Barbalho SM, Goulart R de A, Quesada K, Bechara MD, de Carvalho A de CA. Inflammatory bowel disease: can omega-3 fatty acids really help? Ann Gastroenterol. 2016;29(1):37-43.
14. Ju S, Ge Y, Li P, et al. Dietary quercetin ameliorates experimental colitis in mouse by remodeling the function of colonic macrophages via a heme oxygenase-1-dependent pathway. Cell Cycle. 2018;17(1):53-63. doi:10.1080/15384101.2017.1387701
15. Burge K, Gunasekaran A, Eckert J, Chaaban H. Curcumin and Intestinal Inflammatory Diseases: Molecular Mechanisms of Protection. Int J Mol Sci. 2019;20(8). doi:10.3390/ijms20081912
16. Salaritabar A, Darvishi B, Hadjiakhoondi F, et al. Therapeutic potential of flavonoids in inflammatory bowel disease: A comprehensive review. World J Gastroenterol. 2017;23(28):5097-5114. doi:10.3748/wjg.v23.i28.5097
17. Puckett S. Flavonoids – a Powerful Prebiotic for Inflammatory Bowel Disease | IBDCoach. Published January 23, 2022. Accessed October 22, 2023. https://ibd.coach/flavonoids-prebiotic/
18. Jafarzadeh E, Shoeibi S, Bahramvand Y, et al. Turmeric for Treatment of Irritable Bowel Syndrome: A Systematic Review of Population-Based Evidence. Iran J Public Health. 2022;51(6):1223-1231. doi:10.18502/ijph.v51i6.9656
19. Ng QX, Soh AYS, Loke W, Lim DY, Yeo WS. The role of inflammation in irritable bowel syndrome (IBS). J Inflamm Res. 2018;11:345-349. doi:10.2147/JIR.S174982
20. Chlebicz-Wójcik A, Śliżewska K. Probiotics, Prebiotics, and Synbiotics in the Irritable Bowel Syndrome Treatment: A Review. Biomolecules. 2021;11(8):1154. doi:10.3390/biom11081154
21. Satish Kumar L, Pugalenthi LS, Ahmad M, Reddy S, Barkhane Z, Elmadi J. Probiotics in Irritable Bowel Syndrome: A Review of Their Therapeutic Role. Cureus. 14(4):e24240. doi:10.7759/cureus.24240
22. Jakubczyk D, Leszczyńska K, Górska S. The Effectiveness of Probiotics in the Treatment of Inflammatory Bowel Disease (IBD)—A Critical Review. Nutrients. 2020;12(7):1973. doi:10.3390/nu12071973
23. Bibiloni R, Fedorak RN, Tannock GW, et al. VSL#3 probiotic-mixture induces remission in patients with active ulcerative colitis. Am J Gastroenterol. 2005;100(7):1539-1546. doi:10.1111/j.1572-0241.2005.41794.x
24. Puckett S. Fiber for Inflammatory Bowel Disease: Influential Gut-Friendly Prebiotic | IBDCoach. Published January 20, 2022. Accessed October 22, 2023. https://ibd.coach/fiber/
25. González-Gallego J, García-Mediavilla MV, Sánchez-Campos S, Tuñón MJ. Anti-inflammatory, Immunomodulatory, and Prebiotic Properties of Dietary Flavonoids. In: Polyphenols: Prevention and Treatment of Human Disease. Elsevier; 2018:327-345. doi:10.1016/B978-0-12-813008-7.00028-X
26. Chitnavis MV, Braly KL. The Specific Carbohydrate Diet in Inflammatory Bowel Disease: The Evidence and Execution. Pract Gastroenterol. Published online 2019:7.
27. Wang J, Yang P, Zhang L, Hou X. A Low-FODMAP Diet Improves the Global Symptoms and Bowel Habits of Adult IBS Patients: A Systematic Review and Meta-Analysis. Front Nutr. 2021;8:683191. doi:10.3389/fnut.2021.683191
28. Achamrah N, Déchelotte P, Coëffier M. Glutamine and the regulation of intestinal permeability: from bench to bedside. Curr Opin Clin Nutr Metab Care. 2017;20(1):86-91. doi:10.1097/MCO.0000000000000339
29. Chen J, Vitetta L. Butyrate in Inflammatory Bowel Disease Therapy. Gastroenterology. 2020;158(5):1511. doi:10.1053/j.gastro.2019.08.064
30. Karner M, Kocjan A, Stein J, et al. First Multicenter Study of Modified Release Phosphatidylcholine “LT-02” in Ulcerative Colitis: A Randomized, Placebo-Controlled Trial in Mesalazine-Refractory Courses. Am J Gastroenterol. 2014;109(7):1041-1051. doi:10.1038/ajg.2014.104
31. Shafran I, Burgunder P, Wei D, Young HE, Klein G, Burnett BP. Management of inflammatory bowel disease with oral serum-derived bovine immunoglobulin. Ther Adv Gastroenterol. 2015;8(6):331-339. doi:10.1177/1756283X15593693
32. Deters A, Zippel J, Hellenbrand N, Pappai D, Possemeyer C, Hensel A. Aqueous extracts and polysaccharides from Marshmallow roots (Althea officinalis L.): cellular internalisation and stimulation of cell physiology of human epithelial cells in vitro. J Ethnopharmacol. 2010;127(1):62-69. doi:10.1016/j.jep.2009.09.050
33. El-Abhar HS, Hammad LNA, Gawad HSA. Modulating effect of ginger extract on rats with ulcerative colitis. J Ethnopharmacol. 2008;118(3):367-372. doi:10.1016/j.jep.2008.04.026
34. Joo YE. Natural Product-Derived Drugs for the Treatment of Inflammatory Bowel Diseases. Intest Res. 2014;12(2):103-109. doi:10.5217/ir.2014.12.2.103
35. Zhang C, Huang Y, Li P, Chen X, Liu F, Hou Q. Ginger relieves intestinal hypersensitivity of diarrhea predominant irritable bowel syndrome by inhibiting proinflammatory reaction. BMC Complement Med Ther. 2020;20(1):279. doi:10.1186/s12906-020-03059-3
36. Alammar N, Wang L, Saberi B, et al. The impact of peppermint oil on the irritable bowel syndrome: a meta-analysis of the pooled clinical data. BMC Complement Altern Med. 2019;19. doi:10.1186/s12906-018-2409-0
37. Gonsalkorale WM, Miller V, Afzal A, Whorwell PJ. Long term benefits of hypnotherapy for irritable bowel syndrome. Gut. 2003;52(11):1623-1629.
38. Goldenberg JZ, Brignall M, Hamilton M, et al. Biofeedback for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2019;2019(11):CD012530. doi:10.1002/14651858.CD012530.pub2
39. Bonaz B. Anti-inflammatory effects of vagal nerve stimulation with a special attention to intestinal barrier dysfunction. Neurogastroenterol Motil. 2022;34(10):e14456. doi:10.1111/nmo.14456
40. Fornaro R, Actis GC, Caviglia GP, Pitoni D, Ribaldone DG. Inflammatory Bowel Disease: Role of Vagus Nerve Stimulation. J Clin Med. 2022;11(19):5690. doi:10.3390/jcm11195690